
Newsletter
- [ Vol. 1 No. 1 ]
(January - April 2000 ) - [ Vol. 1 No. 2 ]
(May - August 2000 ) - [ Vol. 1 No. 3 ]
(September - December 2000 ) - [ Vol. 2 No. 2 ]
(May - August 2001 ) - [ Vol. 2 No. 3 ]
(September - December 2001 ) - [ Vol. 2 No. 1 ]
(January - April 2001 ) - [ Vol. 3 No. 1 ]
(January - April 2002 )
 1 of 5
1 of 5

Newsletter
[ Vol. 13 No. 1 ] (January - April 2012 )
Bloodstream infections associated with parenteral nutrition preparation methods in the united states: A large database analysis of infection rates
Robin S. Turpin
Global Health Economics, IV Nutrition, Baxter Healthcare (United States)
Introduction: Bloodstream infection (BSI) is a common cause of morbidity and mortality in hospitalized patients in the United States, with mortality rates reported at 12-25%.1 Furthermore, BSIs add substantial financial burden due to longer hospital stays, medication use, and medical procedures. A recent cohort study among patients with central venous catheters found that PN was an independent risk factor for BSI.2 Among Parenteral nutrition (PN) patients, BSI rates have been reported to vary from 1.3% to 39%.3,4
In the U.S., PN may be delivered via custom-compounding (CPN) or commercial pre-mix multi-chamber bag (MCB), but until recently little has been known about potential differences in clinical outcomes between these delivery systems. The presentation proposed to the PENSA organizing committee will describe several published papers that detail the analysis of a large U.S. retrospective database (PREMIER Study).5,6,7 These papers:
- Report BSI rates in a large PN hospitalized population to determine if delivery system (CPN vs. MCB) was associated with different BSI rates, and
- Evaluated whether the addition of lipid emulsion was associated with a higher risk for infection.
Additional information will be presented that:
- Compares hospital direct and avoidable costs to determine whether CPN or MCB provides increased cost effectiveness through a lower infection risk, and
- Describes preliminary data from a newly completed chart review study in Germany exploring the clinical outcomes associated with MCB, CPN and open-bottle PN delivery systems (ENTREPRENEUR Study).
Methods: In the PREMIER study, inpatient data from a nationally representative hospital network database managed by Premier Healthcare Alliance were analyzed. The Premier Perspective comparative hospital database covers more the 400 hospitals and contains a total of 2.5 billion patient daily service records, with about 45 million records added each month. Data analysis included all hospitalized patients 18 years of age and older who received PN from January 1, 2005 to December 31, 2007. Patients were classified as receiving PN via either MCB (manufactured PN in a dual-chamber bag with dextrose and amino acids, which may have included additions of minerals, vitamins, and/or electrolytes) or CPN (either hospital compounded or outsourced). Patients received their PN either with supplemental soybean oil-based lipid emulsion or without; lipids were administered either through a separate line or piggybacked through the PN line. Since bacterial infection, hepatic dysfunction, hypoglycemia, acute cholecystitis, phlebitis, thrombophlebitis, and pulmonary embolism were identified as either primary or secondary outcomes, patients admitted with those diagnoses were excluded from the analysis. We examined BSI rates as our primary dependent variable, which was defined as the occurrence of ICD-9 codes of 038.x (septicemia), 995.91 (sepsis), 995.92 (severe sepsis), or 790.7 (bacteremia). Hospital variables examined were bed size, teaching status, geographic region, and metropolitan location. Patient characteristics included age, gender, ethnicity, comorbidities (i.e., malnutrition, intestinal malabsorption, acute pancreatitis, peritonitis, gastrointestinal fistula, Crohn’s disease, cancer, cirrhosis or chronic liver disease, renal failure, diabetes mellitus, and tuberculosis), All Patient Refined Diagnosis Related Group (APR-DRG) Severity Class, and surgical, admission and discharge status. PN treatment included days of PN, prior admission of PN, and daily PN volume. Economic outcomes included hospital length of stay (LOS), use of intensive care unit (ICU) and ICU LOS, and total hospital costs.
Analysis: Independent t-tests were used to compare continuous variables of the MCB and CPN groups. Two-group z-tests compared observed BSI and mortality rates for the MCB and CPN groups. Multivariate logistic regression was used to create a model to calculate adjusted rates of BSIs per group and estimate the risk if BSI and mortality. This model included 29 variables that adjusted for baseline differences, risk factors and potential confounders in the database, as listed above. In addition, as a sensitivity analysis we utilized propensity score modeling to create matched groups of patients receiving MCB and CPN and performed similar outcome assessments.
Findings: In the overall analysis, there were 4,669 patients who received MCB and 64,315 who received CPN. For the propensity analysis, the final matched groups consisted 3,048 PN patients (n=1,524 MCB, n=1,524 CPN). The final sample for the lipid analysis was 4,669 patients; 2,023 without lipids and 2,646 with lipids.
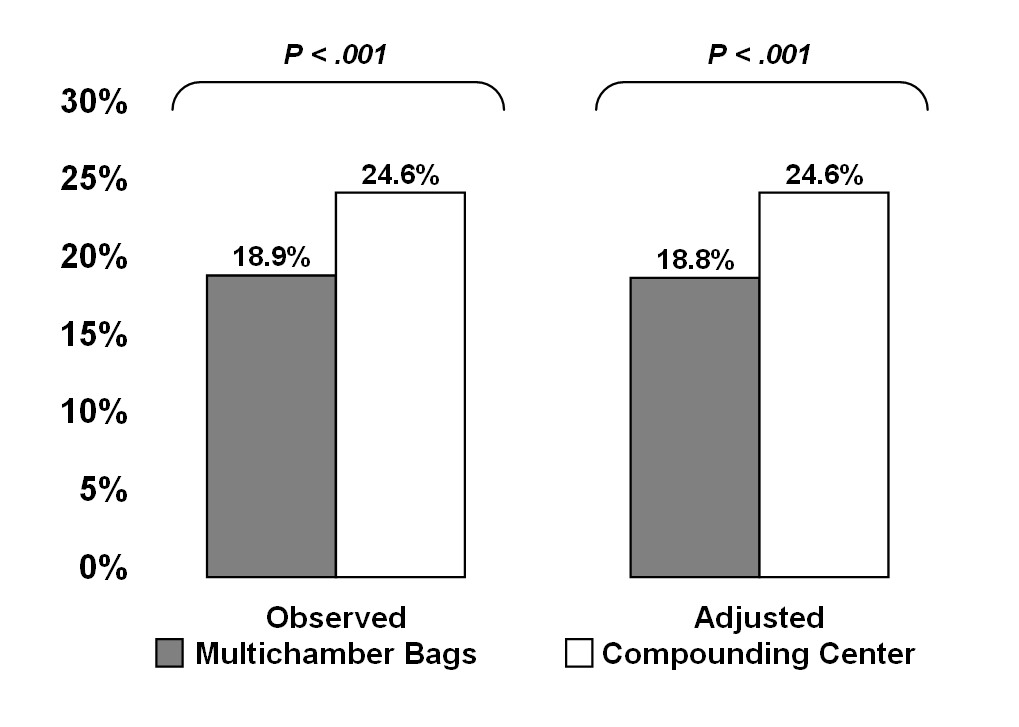
The observed BSI rate in the MCB group was 17.5%, significantly lower than that of the CPN group (26.6%; P<.001). Our model utilized the 29 hospital, patient and PN variables previously described to control for identifiable risk factors, and calculated BSI rates to adjust for any observed differences in risk between the groups. After adjustment, the BSI rate was still significantly different for the two groups (19.6% vs. 25.9%, P<.001; OR = 1.54, 95% CI 1.39 to 1.69). These results are presented in Figure 1. Similar results were found for the propensity matched group analysis (Figure 2). In-hospital mortality for the MCB group was 15.2% vs. 18.9% for the CPN group (p < 0.001). The mean length of stay (LOS) for CPN was 7.3 days longer than the MCB group (days adjusted for baseline differences). In the lipid comparison, the probability of any infection in the overall study population was no different between the groups with or without lipids (OR 1.11, 95% CI 0.96-1.26).
Discussion and Conclusions: Though there are several limitations associated with this study, our analysis is one of the first reports describing PN patients and associated BSI rates in the real-world setting. Our analyses indicate that patients who received MCB were treated in smaller, non-teaching hospitals. Patients receiving MCB also tended to be older, female, and on public funding, with a longer length of stay and less apparent disease acuity. This lower severity may, in part, explain the lower inpatient mortality rate among MCB patients, as well as the shorter duration of hospitalization, fewer PN days, and lower rates of BSI. However the severity was no different between observed and adjusted BSI rates in the propensity score matched groups suggesting that something other than severity contributed to the findings.
Once illness severity and other baseline variables were accounted for, the adjusted probability of BSIs remained significantly lower for the MCB than the CPN group. These results were replicated in the propensity matched group analysis. Our analysis also found that the probability of developing and infection or BSI among patients who received premixed PN that included lipid emulsion was not likely associated with an increase in infectious morbidity or mortality. These findings are useful for generating hypotheses for a large scale study, and may provide impetus for individual hospital-focused quality improvement for patient safety, pharmacy compounding practices and infection control initiatives.
References
- Centers for Disease Control and Prevention (CDC). Reduction in central-line associatedbloodstream infection among patients in intensive care units – Pennsylvania – April 2001 – March 2005. MMWR Morb Mortal Wkly Rep. 2005;54;1013-1016.
- Beghetto MG, Victorino J, Teixeira L, Azevedo MJ. Parenteral nutrition as a risk factor for central venous catherer-related infection. JPEN J Parenter Enteral Nutr. 2005;29:367-373.
- Dissanaike S, Shelton M, Warner K, O’Keefe GE. The risk of bloodstream infections is associated with increased parenteral caloric intake in patients receiving parenteral nutrition. Crit Care. 2007;11:R114.
- Opilla M. Epidemiology of bloodstream infection associated with parenteral nutrition. Am J Infect Control. 2008;36:S173.e5-8.
- Pontes-Arruda A, Liu FX, Turpin RS, Mercaldi K, Hise M, Zaloga G. Bloodstream infections in patients receiving manufactured parenteral nutrition with vs. without lipids: Are the new nutrition support guidelines appropriate? Journal of Parenteral and Enteral Nutrition (JPEN), 2011 (in press).
- Mercaldi CJ, Reynolds MW, Turpin RS. Methods to identify and compare parenteral nutrition administered from hospital compounded and premixed multi-chamber bags in a retrospective hospital claims database. Journal of Parenteral and Enteral Nutrition (JPEN), 2011 (in press).
- Turpin RS, Canada T, Rosenthal V, Nitzki-George D, Liu FX, Mercaldi K, Pontes-Arruda P. Bloodstream infections associated with parenteral nutrition preparation methods in the United States: A retrospective, large database analysis. Journal of Parenteral and Enteral Nutrition (JPEN), 2011 (in press).
Figure 1 - Overall Population BSI Rates
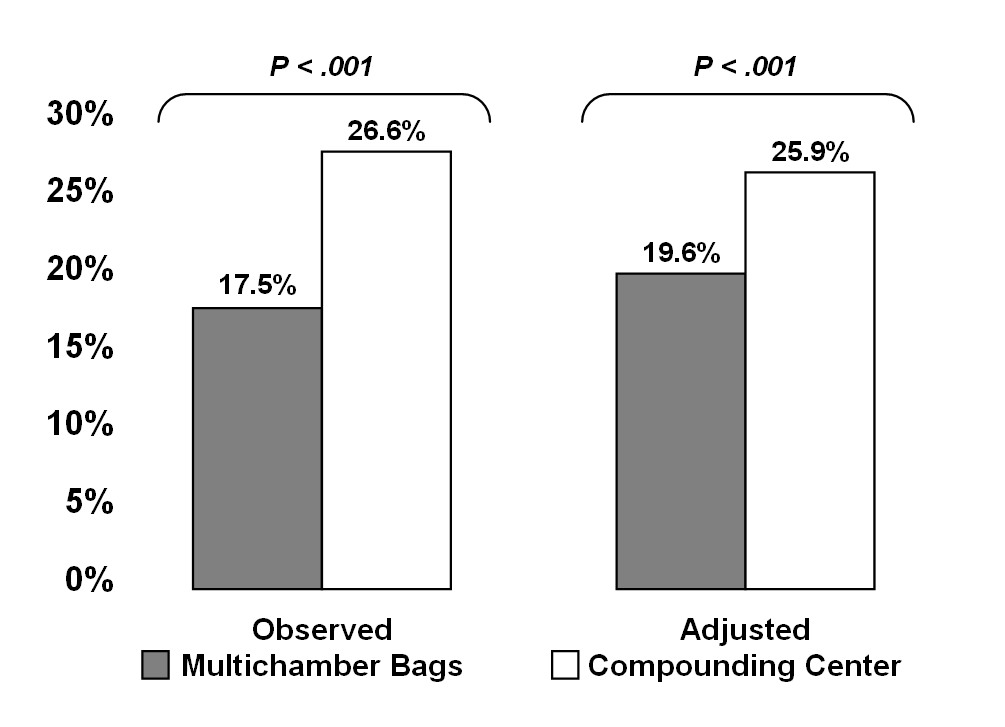
Figure 2 -- Propensity Matched Groups BSI Rates
From
The 14th Congress of Parenteral and Enteral Nutrition Society of Asia
“From Nutrition Support to Nutrition Therapy”
October 14-16, 2011, Taipei, Taiwan
Page: 28-31


